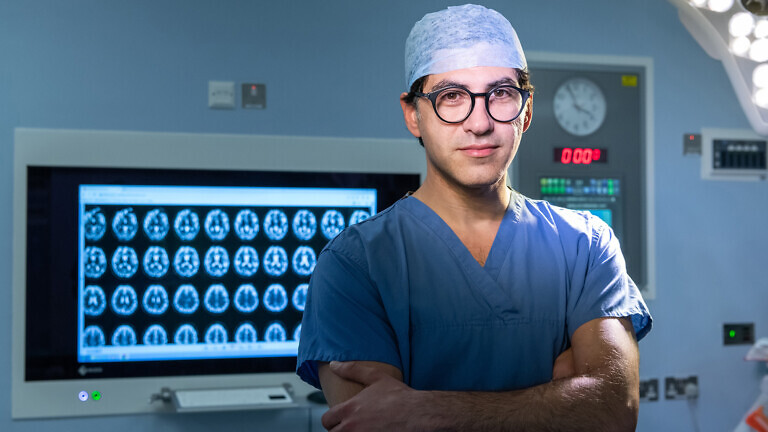
The Scottish Conservative and Unionist Party spokesperson for health and social care explains why healthcare managers should be registered professionals.
The only medical professional in the Scottish parliament – he still works as a GP one day a week – Dr. Sandesh Gulhane is the Scottish Conservative and Unionist Party’s spokesperson for health and social care. Here, he talks to Healthcare Today about why funding for primary care should more than double from 6% to 15% of the NHS budget and why managers within the healthcare system should be enablers rather than gatekeepers.
You’re the only medical doctor in Holyrood and health spokesperson for the Scottish Conservatives. How do you characterise your party’s vision for the NHS in Scotland?
I envision a healthcare system that is modern, efficient, locally delivered, and universally accessible. Achieving this vision requires fundamental changes across several key areas.
Modernisation demands the full integration of technology into our services. We must extend digital healthcare across Scotland while shifting our focus from reactive treatment to proactive disease prevention.
Localisation is critical when we consider that 85-90% of patient interactions occur in primary care. Rather than concentrating on hospitals – which most people rarely need – we should strengthen community healthcare. Our policy will involve doubling primary care funding from 6% to 12% of the NHS budget, rising to 15% by the end of the parliamentary term. This investment will create a responsive primary care service that reduces unnecessary hospital visits and out-of-hours demand by ensuring timely GP access.
Efficiency requires embracing innovation while addressing structural issues. We’ll implement AI and technology to improve service delivery, particularly for remote communities who shouldn’t need to travel to Edinburgh for care. The NHS currently suffers from excessive, siloed management – we need leaner structures with greater accountability. Protecting underperforming managers must stop; we require an agile NHS capable of rapid adaptation.
Finally, we must foster collaboration through a quadruple helix approach – uniting universities, innovative private sector partners, the NHS and, crucially, patients themselves. Only through this coordinated effort can we deliver the modern, efficient and locally responsive service Scotland deserves.
“Doctors are left to carry the burden, while management is insulated”
The SNP constantly blames Westminster austerity for pressure on the NHS, while your party argues it’s mismanagement. Where do you believe the primary responsibility lies?
Let’s consider the scandal at the Queen Elizabeth University Hospital in Glasgow. Who has been held accountable or dismissed? Not a single person. We could look at virtually every scandal in the NHS, and the pattern is the same: not one manager has ever been held accountable.
We submitted a Freedom of Information request, which revealed that in the past five years, fewer than five complaints have been made against NHS managers. As a doctor, I know that complaints are inevitable if you’re doing enough work. That is the unfortunate but undeniable reality of medicine.
Why is it that NHS managers are not receiving complaints? Doctors are left to carry the burden, while management is insulated.
This points to a deeper structural issue within the NHS. We have senior clinicians and we have management, but the two operate in separate silos. What we desperately need is a complete overhaul – a rethinking of how workflows are structured and where accountability lies.
The current culture suggests that if you’re an NHS manager, your position is essentially a job for life. I’ve personally seen a manager perform so poorly that we were explicitly told not to cause any fuss – because they were being lined up for a promotion and would soon be leaving the trust. That’s the system: poor managers are promoted rather than disciplined.
The government has the authority to dismiss board members and managers but it doesn’t because of the cosy relationship between senior management and government. It’s a mutual protection pact: “I protect you; you protect me”.

We can’t get away from the fact that the NHS workforce remains under pressure. What would a Conservative-led strategy do differently to retain and recruit staff across primary and secondary care?
It’s about the culture. We need a complete cultural shift from the top down. Managers shouldn’t see themselves as being in charge. They should act as facilitators. We need enablers in management, not gatekeepers.
We should be making small, inexpensive changes that have a huge impact. Reintroduce common rooms so doctors can decompress. Hire one extra nurse per theatre to allow staff to take proper breaks – those breaks save hours each day in efficiency. Give operating theatres an extra porter so patients arrive on time. These are simple changes, and they cost very little. But management thinks these are areas where savings can be made.
“Instead of investment, we’re piling pressure onto general practice”
BMA Scotland has raised concerns about a £290 million shortfall in general practice funding. Do you accept that figure?
General practice is the cheapest form of healthcare in the world. From a business perspective, if your most frequently accessed service is also the most cost-effective, what should you do? You invest in it. It’s basic logic – yet we’re doing the opposite.
Instead of investment, we’re piling pressure onto general practice. The rise in National Insurance contributions is crippling GP practices.
The baseline funding for GPs is under serious strain and general practice is in trouble. We have trained GPs who are unemployed, and at the same time, patients can’t get an appointment.
We need to invest properly in primary care. That’s why I would commit to allocating 12% of the NHS budget to primary care – rising to 15% over the course of the next parliament. That investment will lead to savings across the whole NHS system.
But this isn’t just about primary care. Our hospitals also need to become more efficient. I don’t think it’s acceptable for a hospital to receive a set amount of funding for operations, without any accountability for how much they actually do. We need to move towards a model where funding follows the patient.

What role do you see for private providers within the NHS in Scotland? Is there space for expanding their role under Conservative policy?
There will always be a market for private healthcare. Even when there are no significant NHS waiting times, some people still choose to go private. That market will always exist.
But what I want is a system where the average person never feels they have to consider going private. We’re British – we understand the concept of a queue. If you tell someone they need a hip replacement and that they’re on a waiting list, most people are fine with that. All they want to know is: how long is the wait?
We need to move to a position where waiting times are fair and manageable. That principle should apply across the board: for GP appointments, for out-of-hours services, for routine outpatient clinics. The standard must be that the wait is tolerable, not endless.
The same applies to people in remote and island communities. No one living on an island expects to have a world-leading neurosurgeon on their doorstep. But they do expect to see a doctor when they need one.
“We need to establish a culture where secrecy is treated as a disciplinary issue”
In your recent comments to The Scotsman, you called medical negligence payouts in Scotland “eye-watering”. What policy change are you advocating in response?
Mistakes happen. If you do enough surgery, you will experience complications. It’s inevitable. I once had a patient die on the operating table while I was performing surgery.
It was devastating for me, for the family – and of course, for the patient. But when complications occur, you must be honest. You must go and speak to the family, be open, and explain exactly what happened.
I didn’t receive a complaint about that case because we were honest. We explained how it had happened, what we did, and I offered my sincere regret and apology. Most complaints don’t stem from the incident itself – they come from the absence of an apology. It’s secrecy that breeds mistrust.
The second issue is the pressure we put our clinicians under. We have to ensure that the environment we ask our staff to work in is as safe as it can be. That means no 15-hour waits. That means not bombarding staff with constant interruptions. We need a system that’s fit for purpose. We need our nurses to do the jobs they’re trained to do. And we need to give them the time and space to do those jobs properly.
When Healthcare Today talked to Jeremy Hunt earlier this year he was proud of bringing “duty of candour” into the NHS. Why is it taking so long to filter through?
If you start from a place of secrecy, it spreads throughout every level of your organisation.
We need to establish a culture where secrecy is treated as a disciplinary issue. I’m regulated by the General Medical Council (GMC); nurses are regulated by the NMC; but who regulates the managers?
Managers should be registered professionals. They should have a registration number, just like doctors and nurses. And that registration should come with responsibilities, just as mine does under the GMC.
Once you create that kind of framework, you give people the ability to raise legitimate concerns.