Although women across England will be offered home-testing kits as part of the cervical screening programme, some say that it doesn’t go far enough.
The government has said that women in England who haven’t come forward for vital health checks will be offered home-testing kits as part of the cervical screening programme under the upcoming 10 Year Health Plan.
The plan aims to tackle barriers that keep some women away from screenings, including a fear of discomfort, embarrassment, cultural sensitivities and the struggle to find time for medical appointments.
Participation in cervical cancer screening currently sits at 68.8%. This is below the NHS England target of 80%. Experts believe this targeted approach could increase participation in the screening programme.
The programme specifically targets those groups which consistently miss vital appointments such as younger women, ethnic minority communities facing cultural hurdles, people with a disability and LGBTQ+ people.
“Screening is a powerful tool to prevent cervical cancer and save lives, but we know it isn’t always easy for everyone to take part,” said Michelle Mitchell, chief executive of Cancer Research UK.
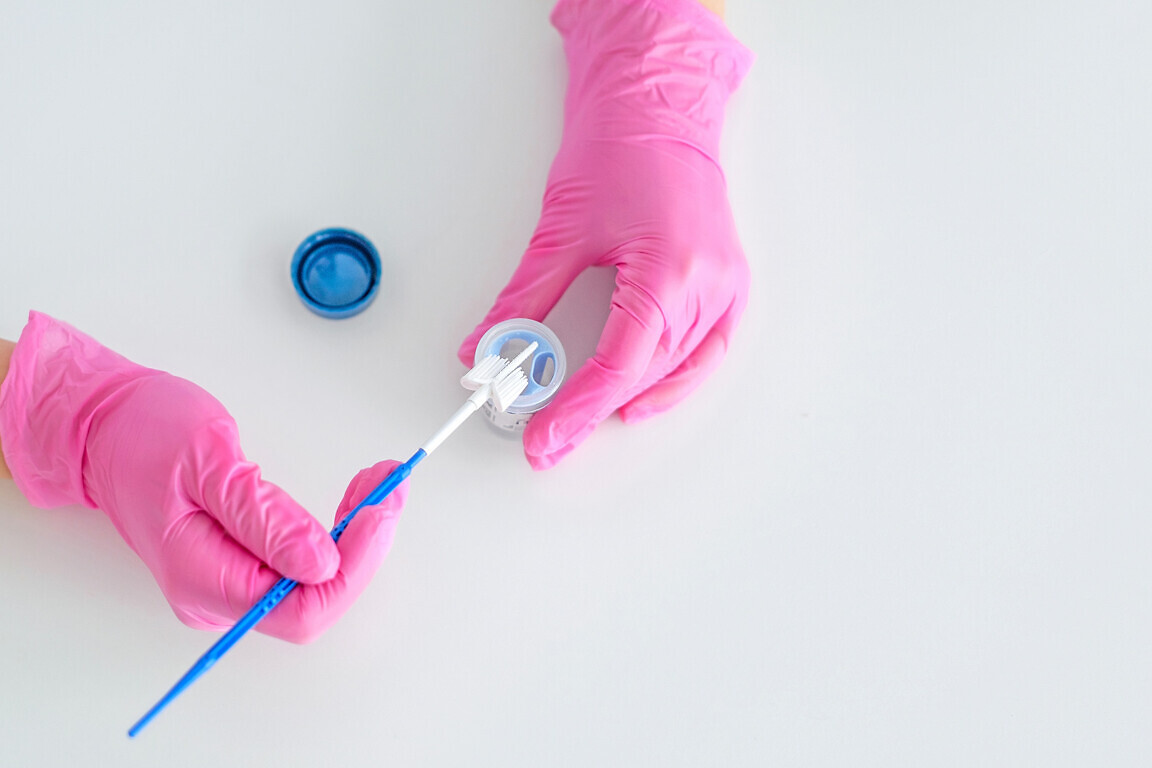
Women who have rarely or have never attended their cervical screening will be offered a self-sample kit to complete at home. They are then sent out in discreet packaging and returned via pre-paid mail.
Women’s health needs do not stop at retirement
The move builds on changes the government announced in late June to cervical screening. Thanks to more accurate human papillomavirus (HPV) testing, invitations for screening will be sent out every five years instead of every three for women aged 25-49 in England, if they have a negative test.
The proposed age range for at-home testing kits of 25-34 is welcome, but concerns remain around ensuring consistent uptake and engagement.
“We strongly welcome this important step forward in empowering women to take charge of their own health,” said Ruth Healey, President of Soroptimist International Great Britain and Ireland (SIGBI). “Making cervical screening more accessible and less invasive has the potential to save countless lives by encouraging earlier detection and treatment.
“With only 68.8% of women currently attending cervical screenings, and with the largest untested group comprising 25 to 34-year-old women, this initiative could play a vital role in increasing screenings for HPV – and therefore saving women from developing cervical cancer.
“However, our concern is that at-home-testing kits are only going to be provided to those women who have a history of not taking up their screening appointments. This could result in women who are routinely attending their appointments, now waiting until self-testing becomes available to them, thereby putting themselves at potential risk.
“We’re keen for public health policy to strike the right balance to protect the health needs of all women. Consistent education on cervical screening and awareness of all testing options will be essential.”