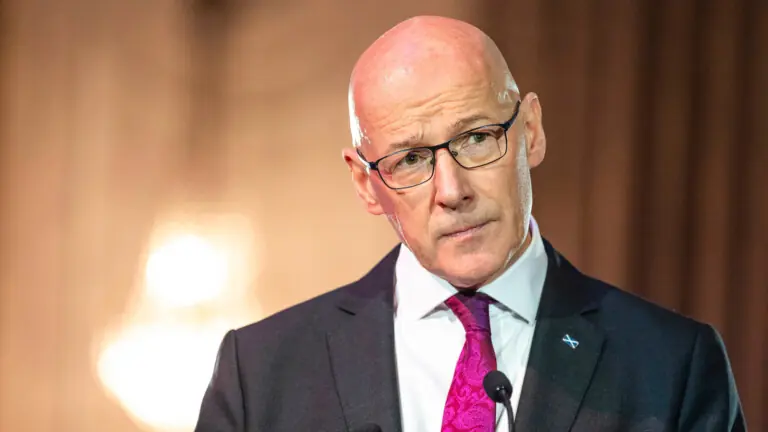
Dr. Beth Walker offers some advice to doctors when discovering their patient is someone they’ve met in the ‘real world’.
With an increasing number of patients turning to the private sector, this scenario may become more common for independent clinicians. The General Medical Council (GMC) makes clear in paragraph 97 of ‘Good Medical Practice’ that doctors must avoid providing medical care to anyone with whom they have a close personal relationship wherever possible. The same principle also applies to prescribing as set out in paragraph 67 of the GMC’s ‘Good practice in prescribing and managing medicines and devices’ guidance.
Defining a ‘close personal relationship’ can sometimes be difficult and will need to be considered, and justified, based on the individual circumstances. Such a relationship may encompass not just family and friends but also colleagues and some acquaintances for example. Even if you do not consider your relationship with the patient you know to be a close personal one, a key question to ask yourself is whether you can be objective. There is a significant risk that a personal relationship can interfere with your clinical judgement and introduce a conflict of interest, such as if you are put under pressure by the patient to provide a particular treatment or if it is challenging to be impartial about their need for it.
Another potential pitfall is that you may find yourself either consciously or subconsciously considering the patient’s convenience or comfort over and above your usual systematic and balanced approach. It may be more difficult too for the patient to be open and honest with you about their symptoms and medical history in these circumstances, which could impact on your ability to provide safe care. There may be an impact on the existing relationship, such as if a problem arises or a risk of blurred boundaries if the patient seeks ad-hoc advice outside of the clinical setting. It is also important to be mindful of the potential for a conflict of interest, or what could be perceived as a conflict, regarding charges and fees.

It is wisest to have a very low threshold in considering if you can be completely objective and to avoid treating someone you know even distantly due to the risks described. If you are referred a patient who you are close to, or a patient who you may not have a close personal relationship with but where you cannot be sufficiently objective, it is advisable to highlight this as soon as possible and arrange for a colleague to see them instead/signpost them to an appropriate alternative service. If there is no alternative, you should keep detailed records to show you have acted in line with good practice and professional guidance and that you can justify any investigations or treatments you put in place. In the event you assess you can be sufficiently objective, you may still wish to seek the patient’s views on whether they feel comfortable seeing you or would prefer to see another colleague if possible.
The GMC gives guidance on what steps you must take if you do prescribe for someone close to you. These principles extend to all aspects of medical care, and not just prescribing. Again, even if you assess you do not have a close personal relationship with the patient, if you decide to treat or prescribe for someone you know, it is safest to follow this guidance. You must keep a careful record of what you did and your reasoning, the nature of your relationship with the patient and the reason it was necessary for you to prescribe. You should have sufficient and reliable information about the patient’s health and other treatments they may be receiving (such as through access to their medical records, through your own examination or testing etc) to ensure you can prescribe safely and meet the patient’s needs. You should also seek the patient’s consent to contact their GP and/or other treating doctors if you need more information to prescribe safely and to share information with their GP about the episode of care you have provided.
If the patient objects to information being shared with you, the GMC advises you must be able to justify that you are able to safely prescribe without that information. If the patient refuses their consent for you to share information with their GP, you should explain to them the risks of not doing so. Further, if you assess that failing to share information could pose a patient safety risk then you should explain that you cannot prescribe and signpost them to appropriate alternative services. The reasoning for any decisions made as part of these considerations should be clearly documented in the patient’s record.
Unsurprisingly, the GMC places even stricter safeguards on prescribing controlled drugs for someone close to you due to the risks of addiction and misuse. It states you must not prescribe them unless there is no alternative prescriber and immediate emergency treatment is necessary to avoid serious deterioration in health or serious harm. Any treatment of those close to you involving medicines at risk of abuse, or where medicines have an effect on the patient’s mental health, would be very difficult to justify before the GMC. However, it should be remembered that there are dangers with any medications, not just controlled drugs, such as unexpected drug interactions and inadequate communication with the patient’s GP.
An exception to avoiding treating or prescribing for someone close to you is in the event of an emergency when all other routes are unavailable, such as the patient’s own GP, the out-of-hours services (for example 111 and urgent care centres) and the emergency department. In the rare circumstance that you find yourself in such a situation, you should ensure you follow the relevant GMC guidance on prescribing for someone close to you and that you can justify that your actions were in the patient’s best interests. It is important to be cognisant that convenience and best interests are not the same thing, though patients can sometimes confuse the two.
Every year, a significant number of doctors are reported to the GMC for prescribing for someone they know. Pharmacists are vigilant to this issue and will copy to the GMC any prescription they have concerns about. Simpler cases may be resolved by providing a clear explanation of what occurred, evidence that the actions were reasonable and in line with good practice, and confirmation that the doctor understands their professional duty in this regard. However, there remain a significant number of cases where the doctor’s treatment or prescribing for someone close to them raises sufficient concern for the GMC that they investigate more fully and there can be serious penalties.

Learning points:
- The GMC states you must avoid treating and prescribing for someone you have a close relationship with wherever possible.
- In providing good clinical care, you must be able to be completely objective and be able to justify your decisions and actions.
- A personal relationship with a patient is likely to affect your judgement – a lack of objectivity can compromise patient care and pose a professional risk to you.
- If you do treat someone you know, your records must demonstrate that you have acted in accordance with good practice and GMC guidance and that you can justify that any prescription or treatment provided was in the patient’s best interests.
- Treatment of those close to you involving medicines at risk of abuse, or where medicines could affect the patient’s mental health, would be extremely difficult to justify before the GMC.
- If you have any concerns around this issue, always contact your medical defence organisation for advice.
Dr. Beth Walker is a medicolegal consultant at Medical Protection.