An announcement from the first minister about a nationwide network of walk-in GP services seems unlikely to make it out of the conference hall.
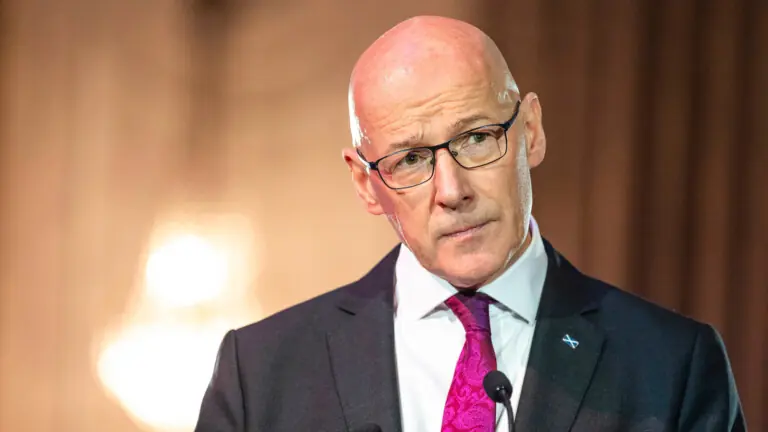
To great fanfare at the SNP party conference in Aberdeen, Scotland’s first minister, John Swinney, announced that his government intended to improve access to primary care. It will create a nationwide network of walk-in GP services which will be open seven days a week, it said.
The clinics, he said during his keynote speech, would tackle the “the 0800 rush for appointments”. Staffed by GPs, nurses and support staff, these services would be open seven days a week from 1200 to 2000. Alongside existing primary care services, they would provide a range of same-day assessments, diagnostics and treatment.
Initially, the new service would be trialled at 15 clinics across the country.
“Improving access to primary care and shifting more care into the community is central for this government,” added health secretary Neil Gray.
“These will be in addition to core GP services and will offer additional flexibility for patients. These will be designed in collaboration with NHS Boards, GPs and other partners to ensure they strengthen existing services,” he continued.
A lack of detail
The plan was almost immediately slammed by the Royal College of General Practitioners (RCGP).
“GPs will have serious concerns about the delivery and impact of this proposal, and we will await clarity on the implementation detail. Who will staff these new services and their extended weekend hours? How will continuity of care be preserved when patients benefit enormously from knowing and trusting their regular GP? Where will these services be located, when many GP practice premises are not fit for purpose and are waiting for long overdue capital investment?” asked Scotland’s RCGP chair Chris Provan.
The best way to deliver improved patient access and care, he continued, would be to provide the level of investment needed to “overcome the impact of cumulative years of underfunding” and the implementation of “a long-term workforce strategy to increase the number of GPs”.
As Healthcare Today reported earlier this year, GPs in Scotland are already struggling to cope with their workload, and nearly half have said that the future of their practice is precarious or unsustainable.
“We need a radical change of approach as to how [the government] supports general practice,” said Iain Morrison, chair of the BMA’s Scottish general practitioners committee, at the time.
Certainly, relations between doctors and the government remain at an all-time low, with a strike ballot planned for resident doctors after what Chris Smith, chair of the BMA’s Scottish Resident Doctor Committee, calls “years and years of being undervalued and under-appreciated”.