Tom Oakley, chief executive of Feedback Medical, argues that the NHS needs the leadership and the ambition to embrace collaboration and reimagine what outpatient care can be.
The traditional outpatient model, which was largely designed in the 1940s and 1950s, is broken. For years, patients have endured lengthy waits, unnecessary appointments, and fragmented care that fails to meet the demands of a modern healthcare system supporting an ageing and expanding population with increasingly complex needs. With challenging productivity targets for NHS providers to meet, funding constraints and workforce challenges, doing more of the same won’t improve the experience for patients. But transformation is not just possible – it’s already happening.
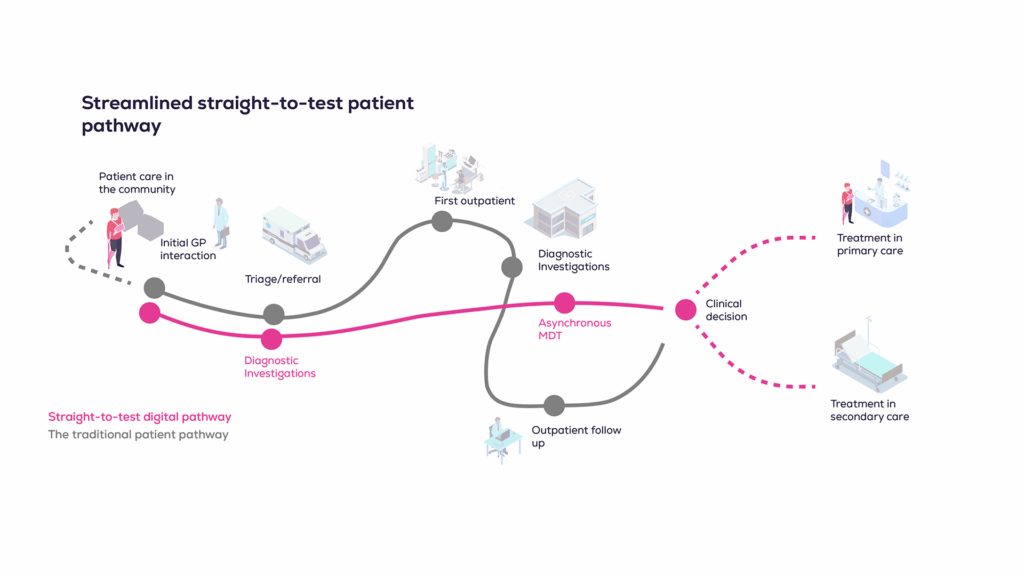
Some forward-thinking NHS systems and providers are redesigning their delivery of outpatient care to flexible, asynchronous, and digitally enabled patient pathways. At the heart of this transformation is a single, radical idea: flip the pathway. Instead of referring a patient, waiting for a specialist visit, ordering diagnostics, and then reviewing results weeks later, why not start with the diagnostics?
Straight-to-test pathways
This straight-to-test model, championed in the government’s reforming elective care plan, challenges the very foundation of outpatient care. By front-loading tests and making them accessible via digital collaboration platforms, clinicians can make informed decisions faster – often without ever needing to see the patient in person. At the Queen Victoria Hospital NHS Foundation Trust in Sussex, this model for its breathlessness pathway has delivered impressive results: 90% of patients have been diverted away from traditional outpatient appointments, wait times have reduced by up to 63% compared to the national referral to treatment target (from 18 to 6.6 weeks), and consultation times have shrunk from 30 minutes to under ten minutes.
This approach could allow a trust to see a 34% wait list reduction in-year if 50% of consultant programmed activity (PA) sessions were delivered asynchronously. For integrated care boards and trusts grappling with the mandate to deliver 118% of baseline activity amid intense financial pressures, such efficiency savings are not just desirable, they’re essential.
A connected digital infrastructure
Central to this transformation is the concept of developing a single point of access, enabling seamless patient flow through referral triage and advice and guidance between primary and secondary care, enhanced by diagnostics. It’s underpinned by a unified digital infrastructure connecting care settings. GPs can access specialist input without unnecessary appointments for their patients, and specialists can review full GP records, diagnostic results, and clinical history asynchronously – all in one platform.
The clinical case is compelling. By integrating cardiac and respiratory diagnostics in a single community diagnostic centre visit, followed by asynchronous review by specialists, only 9% of breathlessness patients ended up needing secondary care. The rest were managed in primary care, more quickly and closer to home.
Neighbourhood-level care
This isn’t just theory, it’s something we’ve put into practice. Sussex is in the process of adopting this approach to additional pathways, including non-specific symptoms, and expanding it to more GP practices and additional hospital sites. It exemplifies the future of integrated, neighbourhood-level care: technology-enabled, clinician-designed, and focused on patient outcomes, not just process.
Of course, digital transformation doesn’t come without challenges. Cultural change is the hardest part. Clinicians are rightly cautious, especially with new workflows and platforms that might impact quality and safety. But success stories like Sussex’s breathlessness pathway build trust by demonstrating how it can work in practice. By co-designing pathways with primary and secondary care clinicians, aligning incentives (like advice and guidance payments), and ensuring specialists are giving timely responses, systems can create genuine clinical engagement.

Patient-centred, shared care
Perhaps the most profound benefit is less technical and more outcomes-based: shared care. By enabling asynchronous, multidisciplinary collaboration, we move from siloed care to something more holistic. GPs can query specialists more easily and see where their patient is on their care journey, patients avoid bouncing between appointments, and clinicians – whether in hospitals or in surgeries – are empowered with better data and better tools. Patients no longer need to traverse the NHS’s complex structures, instead this model allows the NHS to operate around the needs and lives of the patient.
If this model were adopted nationally, it could unlock more than £40 million in annual savings per pathway. But more importantly, it would give time back to clinicians to focus on the patients that really need them and deliver efficiency back to a system straining under its own weight.
What the NHS really needs now is scale and the flexibility to build it. The tools are available, the models work – the data proves it. What remains is leadership and the ambition to change: to break away from tradition, embrace collaboration, and reimagine what outpatient care can be.
Now is the time to stop doing more of the same – and start doing things better.