NHS England has announced a significant change to its cervical screening programme – a move that has sparked both discussion and apprehension.
While this update represents important progress in understanding the link between HPV and cervical cancer, we remain committed to keeping women’s health at the forefront.
Let’s take a closer look at exactly what has changed.
Firstly, here’s the background. Around the world, every two minutes, a woman dies from cervical cancer, and even here in the UK, two women a day die from this entirely preventable disease.
Despite this, one in every three women fails to take up their invitation to attend a screening appointment. However, early detection of cell changes through screening can prevent up to 75% of cases.
These statistics highlight why cervical screening remains one of the most vital tools we have in early detection and prevention, and why changes to access and frequency must be carefully considered.
It’s something Soroptimists – our Soroptimist International Great Britain and Ireland (SIGBI) members – find important.
Over the past few weeks, they have been continuing their vital work to prevent cervical cancer by engaging with their communities, talking to women, and raising awareness about the importance of attending cervical screening appointments.
While the future of cervical cancer is ever-changing, Soroptimists are reflective of how far we’ve progressed over the past century.
It’s not widely known that a female Scottish physician and cytologist, called Janet Elizabeth MacGregor, was the one who pioneered the first successful screening trial programme for cervical cancer in the UK. Back in the 1960s, her work helped lead to a significant decrease in women’s deaths from cervical cancer.
In 1963, the British Medical Journal stated the following: ‘cervical cytology has now passed beyond the experimental stage – that cervical cancer could largely be prevented by cytological detection and treatment of a pre-invasive stage’.
The next transformational discovery occurred in 1983/84, when Nobel Laureate in Medicine, Harald Zur Hausen, detected human papillomavirus (HPV) in cervical cancers.
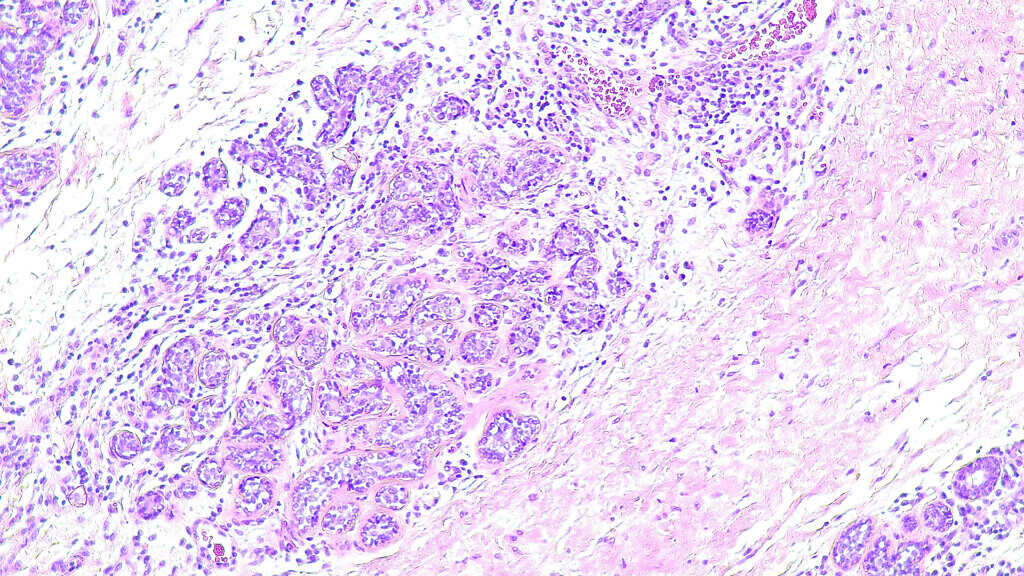
It’s now understood that HPV is responsible for nearly all cervical cancers, so since 2019, all cervical screening samples taken in England have been tested for high-risk HPV. This has been more accurate than the previous method of cytology testing – which in modern terms we know as the traditional ‘smear test’.
In recent years, it has been documented that HPV is also a significant factor in several other cancers, affecting both men and women. The discussion is expanding past being simply a women’s issue, which is not simple at all, but instead to a wider health one.
But back to cervical screening – previously, in England, women were invited for routine cervical screening every three years between the ages of 25 and 49, then every five years until they are 64.
In Scotland and Wales, the screening intervals have already changed for all ages to be invited every five years.
NHS England has announced that from July 1, 2025, all women of screening age (currently 25-64) will be invited every five years in England, unless they are at a greater risk of cervical cancer because of high-risk Human Papilloma Virus (HPV) and or cell changes, when they will be seen more often.
The move follows a recommendation by the UK National Screening Committee, because of research led by King’s College London, which showed that five-yearly screening is as safe as three-yearly, that the same number of cancers are found, and less frequent cervical screening tests are needed.
Studies have shown that if a person tests negative for HPV, they are extremely unlikely to go on to develop cervical cancer within the next decade, leading to the UK National Screening Committee’s recommendation to offer more personalised intervals for women based on their risk.
It was also recently announced that under-screened women will be offered HPV self-testing kits. This is something we’re huge advocates for. We welcome this important step forward in empowering women to take charge of their own health.
Making cervical screening more accessible and less invasive has the potential to save countless lives by encouraging earlier detection and treatment. We hope these tests will help to tackle barriers of embarrassment, discomfort, lack of time, accessibility and religious or cultural concerns for those that are not regularly attending.
With only 68.8% of women currently attending cervical screenings, and with the largest untested group comprising 25 to 34-year-old women, this initiative could play a vital role in increasing screenings for HPV – and therefore saving women from developing cervical cancer altogether.
However, our concern is that at-home testing kits are only going to be provided for those women who have a history of not taking up their screening appointments. This could result in women who are routinely attending their appointments, now waiting until self-testing becomes available to them, thereby putting themselves at potential risk.
Consistent education on cervical screening and awareness of all testing options will be essential.
Other updates have been announced. Following the introduction of a new NHS digital system in England, in 2024, the system has, in the past month, rolled out invitations and reminders for cervical screening via the NHS App, as part of a new ‘ping and book’ service to boost uptake and help save thousands of lives.
Eligible women will first receive a notification through the App to alert them to book a screening appointment, followed by a text message if the App notification isn’t opened. And, as before, letters will remain in place for those who need them.
Dr Sue Mann, NHS National Clinical Director for Women’s Health, has been quoted saying that the NHS is following robust evidence on how women need to be safely screened. She said that by putting invitations and reminders straight in women’s pockets on their phones, they are making it easier than ever to take up screening appointments.
There is always more that can be done, but as an organisation prioritising the needs of women and girls, we’re conscious to celebrate the massive steps forward that have taken place this month.
It’s crucial for decision-makers to prioritise women’s health and improve access for those who aren’t currently attending screenings. By doing so, we can make sure that potentially life-saving cervical cancer testing is truly inclusive and reaches everyone who needs it.
Soroptimist International Great Britain & Ireland (SIGBI), a registered women’s charity founded in 1934, is part of Soroptimist International, a global organisation formed in 1921, born out of the service movement.
The organisation – which has consultancy status at the United Nations – focuses on empowering women and girls to achieve their full potential and works to eliminate barriers and discriminations that hinder women’s progress.
The charity does this through its 248 clubs throughout the UK, Ireland, Malta, Asia and the Caribbean – over 200 of which are in the UK – and currently has a total of 5,150 members.
SIGBI club members are part of a global movement, Soroptimist International, and are united by a desire to advance the lives of women and girls.



